Recent LinkedIn discourse got me thinking of the wider pharmaceutical quality system and how it is reflected in ICH Q10 and in the FDA Guidance for Industry on Quality Systems Approach to Pharmaceutical CGMP Regulation.
ICH Q10
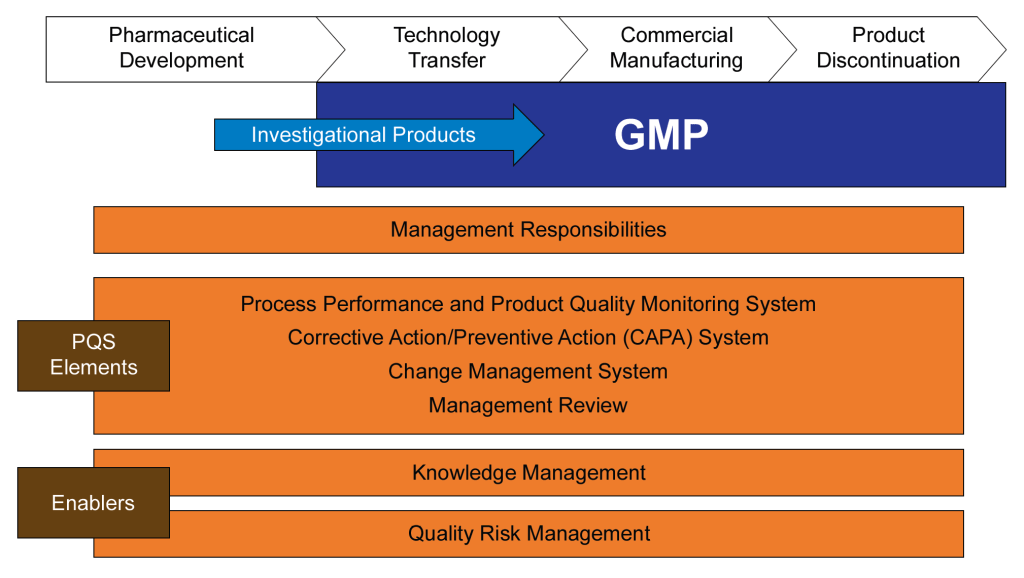
The International Conference on Harmonization (ICH) was established to harmonize the technical requirements for pharmaceutical product registration across Europe, Japan, and the United States. ICH Q10, finalized in June 2008, emerged from this initiative as a guideline for a comprehensive Pharmaceutical Quality System (PQS) applicable throughout the product lifecycle. It was adopted by the FDA in April 2009, following its implementation by the European Commission in July 2008.
ICH Q10 aims to provide a model for pharmaceutical manufacturers to develop and maintain effective quality management systems. The guideline emphasizes a lifecycle approach, integrating quality management principles from ISO standards and regional GMP requirements. The primary objectives of ICH Q10 include:
- Ensuring consistent product quality that meets customer and regulatory requirements.
- Establishing effective monitoring and control systems for process performance and product quality.
- Promoting continual improvement and innovation throughout the product lifecycle.
The guideline outlines the key elements of management responsibilities, Corrective and Preventive Action (CAPA) , process performance and product quality monitoring, change management, and management review. ICH Q10 is usually considered part of the “Quality Trio” with ICH Q8 and Q9. Quality by design is only possible through proper risk management and a robust quality system.
FDA Guidance for Industry on Quality Systems Approach to Pharmaceutical CGMP Regulation
The FDA developed guidance on implementing modern quality systems and risk management practices to align with the CGMP (Current Good Manufacturing Practice) requirements outlined in parts 210 and 211 of the FDA regulations. These regulations govern the manufacturing of human and veterinary drugs, including biological products. Published in 2006, this guidance should be viewed as part of a continuum of thought with ICH Q10 and not as an earlier draft.
This guidance aims to assist manufacturers in meeting cGMP requirements by adopting a comprehensive quality systems model. It emphasizes the integration of quality systems with regulatory requirements to ensure full compliance without imposing new expectations on manufacturers. Key aspects of the guidance include:
- Highlighting the consistency of the quality systems model with cGMP regulations.
- Encouraging the use of risk management and quality systems to enhance compliance and product quality.
- Providing a framework for manufacturers to gain control over their manufacturing processes.
Six-System Inspection Model
The FDA’s Six-System Inspection Model is a framework introduced in this guidance to ensure compliance with current Good Manufacturing Practice (CGMP) regulations in the pharmaceutical industry. This model helps FDA inspectors evaluate the robustness of a company’s quality management system by focusing on six key subsystems.
I am a huge fan of the six subsystem approach. Basically we have here the organization of the quality manual, a guide to what standards you need to write in a bigger company, and a franework for understanding the cGMPs as a whole (great for education purposes).
Here’s a detailed explanation of each subsystem:
1. Quality System
- Role: Acts as the central hub for all other systems, ensuring overall quality management.
- Focus: Management responsibilities, internal audits, CAPA (Corrective and Preventive Actions), and continuous improvement.
- Importance: Ensures that all other systems are effectively integrated and managed to maintain product quality and regulatory compliance.
2. Facilities and Equipment System
- Role: Ensures that facilities and equipment are suitable for their intended use and maintained properly.
- Focus: Design, maintenance, cleaning, and calibration of facilities and equipment.
- Importance: Prevents contamination and ensures consistent manufacturing conditions.
3. Materials System
- Role: Manages the control of raw materials, components, and packaging materials.
- Focus: Supplier qualification, receipt, storage, inventory control, and testing of materials.
- Importance: Ensures that only high-quality materials are used in the manufacturing process, reducing the risk of product defects.
4. Production System
- Role: Oversees the actual manufacturing processes.
- Focus: Process controls, batch records, in-process controls, and validation.
- Importance: Ensures that products are manufactured consistently and meet predefined quality criteria.
5. Packaging and Labeling System
- Role: Manages the packaging and labeling processes to ensure correct and compliant product presentation.
- Focus: Label control, packaging operations, and labeling verification.
- Importance: Prevents mix-ups and ensures that products are correctly identified and used.
6. Laboratory Controls System
- Role: Ensures the reliability of laboratory testing and data integrity.
- Focus: Sampling, testing, analytical method validation, and laboratory records.
- Importance: Verifies that products meet quality specifications before release.
Integration and Interdependence
- Quality System as the Fulcrum: The quality system is the central element that integrates all other subsystems. It ensures that each subsystem functions correctly and is aligned with overall quality objectives.
- State of Control: The primary goal of the six-system inspection model is to ensure that each subsystem is in a state of control, meaning it operates within predefined limits and consistently produces the desired outcomes.
The Six-System Inspection Model provides a structured approach for FDA inspectors to assess the compliance and effectiveness of a pharmaceutical company’s quality management system. By focusing on these six subsystems, the FDA ensures that all aspects of manufacturing, from raw materials to final product testing, are adequately controlled and managed to maintain high standards of product quality and safety.
A Complementary and Holistic Approach
Both ICH Q10 and the FDA’s guidance on quality systems approach aim to enhance the quality and safety of pharmaceutical products through robust quality management systems. ICH Q10 provides a harmonized model applicable across the product lifecycle, while the FDA guidance focuses on integrating quality systems with existing CGMP regulations. Together, they support the pharmaceutical industry in achieving consistent product quality and regulatory compliance.
| Aspect | ICH Q10 | FDA Guidance on CGMP | ISO 13485 and 21 CFR 820 | ISO 9000 |
|---|---|---|---|---|
| Purpose and Scope | Comprehensive model for pharmaceutical quality systems across the product lifecycle. | Quality systems approach to ensure CGMP compliance in pharmaceuticals. | Quality management system for medical devices, incorporating ISO 13485 and regulatory requirements of 21 CFR 820. | Fundamentals and vocabulary for quality management systems applicable to any industry. |
| Industry Focus | Specifically for the pharmaceutical industry. | Specifically for the pharmaceutical industry. | Specifically for the medical device industry. | Applicable to any industry. |
| Key Elements | Management responsibilities, CAPA, process performance, change management, management review. | Management responsibilities, quality systems, process validation, continuous improvement. | Risk management, quality manual, documentation requirements (e.g., Device Master Records, Device History Records). | Quality management principles, terms, and definitions. |
| Regulatory Focus | Strong emphasis on regulatory compliance and lifecycle management. | Strong emphasis on regulatory compliance with CGMP. | Incorporates regulatory requirements specific to medical devices (21 CFR 820). | Does not directly address regulatory compliance. |
| Flexibility | Flexible, adaptable to specific product and process needs. | More prescriptive with specific compliance requirements. | Harmonized with international standards but includes specific regulatory requirements. | Provides a broad framework for customization. |
| Management Involvement | Emphasizes management’s role in quality and regulatory compliance. | Emphasizes management’s role in quality and CGMP integration. | Emphasizes management’s role in quality and risk-based decision making. | Emphasizes management’s role in quality and customer satisfaction. |
| Implementation | Tailored to pharmaceutical manufacturing, integrating quality management principles. | Mandates oversight and controls over drug manufacturing processes. | Requires a quality manual and specific documentation practices; aligned with international standards. | Requires customization to specific industry needs. |
These two documents were developed at the same time and represents the thinking twenty years ago in laying down an approach that still matters today. I usually regard the six system approach as a deepening and defining of what Q10 means by process performance and product quality monitoring.
What is the current agency thinking?
The FDA and other revulatory agencies haven’t stopped their thinking in 2008. Sixteen years later we see the continued push for quality culture and quality maturity. The FDA continues to make this a top priority, as we’ve been seeing in their annual drug shortage reports to Congress. There are a few themes we continue to see driven home.
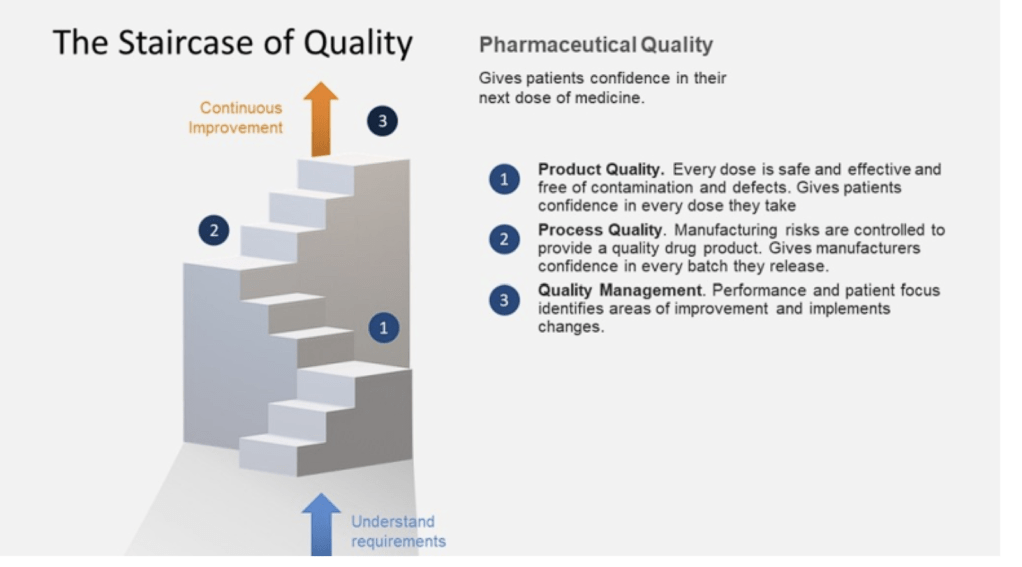
The Patient is the Customer
Quality management must be customer-focused, ensuring that all processes and materials meet their intended use. Senior management’s commitment is crucial for a strong QMS, which emphasizes proactive quality assurance over reactive quality control. Robust supplier relationships and oversight programs are essential to manage variability in materials and processes.
This application of a core priciple in ISO 9000 may seem to basic to some, but I think it is central to a lot of messaging and should never be taken for granted.
Benefits of Better Quality Performance
A continued focus that a quality-focused culture leads to:
- Early problem detection
- Enhanced process stability and productivity
- Fewer major deviations and failures
- Efficient QA release of batches
- Reduced customer complaints and returns
- Protection of brand and competitiveness
Management Oversight of Drug Quality
Management must address sources of variability, including people, materials, methods, measurements, machines, and environment. Risk management should be dynamic and ongoing, facilitating continual learning and improvement.
Corrective Action and Preventive Action (CAPA)
A structured approach to investigating complaints, product rejections, nonconformances, recalls, deviations, audits, regulatory inspections, and trends is essential. CAPA should determine root causes and implement corrective actions.
Change Management
Timely and effective change management ensures corrections and improvements are undertaken efficiently. This includes implementing product quality improvements, process improvements, variability reduction, innovations, and pharmaceutical quality system enhancements.
Management Review
Management is responsible for quality policy, QMS effectiveness, internal communications, resource management, and supply chain oversight. This includes ensuring the quality of incoming materials and outsourced activities.
Quality Culture Driven by Top Management
A strong corporate quality culture is driven by daily decisions and executive oversight. Sustainable compliance requires aiming for high standards rather than just meeting minimum requirements. Quality management maturity involves proactive and preventive actions, iterative learning, and leveraging modern technologies.
Facility Lifecycle
Senior management must ensure the suitability of operational design, control, and maintenance. This includes addressing infrastructure reliability, appropriateness for new product demands, and mitigating equipment/facility degradation.
Risk Management in Manufacturing
Human factors and manual interventions pose significant risks in pharmaceutical manufacturing. Automation and separation technologies can mitigate these risks, but many facilities still rely on manually intensive processes. Leveraging new technologies and practices is a huge opportunity.
This approach is reflected in the FDA’s Quality Management Maturity (QMM), which promotes advanced quality management practices within drug manufacturing establishments.
Goals of the QMM Program
- Foster a Strong Quality Culture Mindset: Encourage establishments to integrate quality deeply into their organizational culture.
- Recognize Advanced Quality Management Practices: Acknowledge and reward establishments that go beyond basic CGMP (Current Good Manufacturing Practices) requirements.
- Identify Growth Opportunities: Provide suggestions for enhancing quality management practices.
- Minimize Risks to Product Availability: Ensure a reliable market supply by reducing quality-related failures and maintaining performance during supply chain disruptions.
Key Components of the QMM Program
- Management Commitment to Quality: Leadership must prioritize quality, set clear objectives, and integrate these with business goals. Effective management review processes are crucial.
- Business Continuity: Establishments should develop robust plans to handle disruptions, ensuring consistent operations and supply chain reliability.
- Advanced Pharmaceutical Quality System (PQS): Implementing quality principles like Quality by Design (QbD) and risk management approaches to maintain system reliability and minimize production disruptions.
- Technical Excellence: Emphasizing data management, innovative manufacturing processes, and advanced technologies to enhance quality and operational efficiency.
- Employee Engagement and Empowerment: Encouraging employees to take ownership of quality, make suggestions, and understand their impact on product quality and patient safety.
Implementation and Assessment
- The FDA has developed a prototype assessment protocol to evaluate QMM. This includes a standardized approach to minimize bias and ensure objectivity. Someday, eventually, it will move away from constant prototyping.
- Assessments will focus on qualitative aspects, such as the establishment’s quality culture and how it uses data to drive improvements.
Benefits of QMM
- Enhanced Supply Chain Reliability: By adopting mature quality management practices, establishments can reduce the occurrence of quality-related failures. The fact shortages continue to be so damning to our industry is a huge wake-up call.
- Proactive Continual Improvement: Encourages a proactive approach to quality management, leveraging technological advancements and integrated business operations.
- Long-term Cost Savings: Investing in a mature quality culture can lead to fewer compliance issues, reduced inspection needs, and overall cost reductions.
Conclusion
The FDA’s QMM program aims to transform how pharmaceutical quality is perceived, measured, and rewarded. The program seeks to ensure a more reliable drug supply and better patient outcomes by fostering a strong quality culture and recognizing advanced practices. It should be seen as part of a 20-year commitment from the agency in alignment with its international partners.




