The Catalent Indiana 483 form from July 2025 reads like a textbook example of my newest word, zemblanity, in risk management—the patterned, preventable misfortune that accrues not from blind chance, but from human agency and organizational design choices that quietly hardwire failure into our operations.
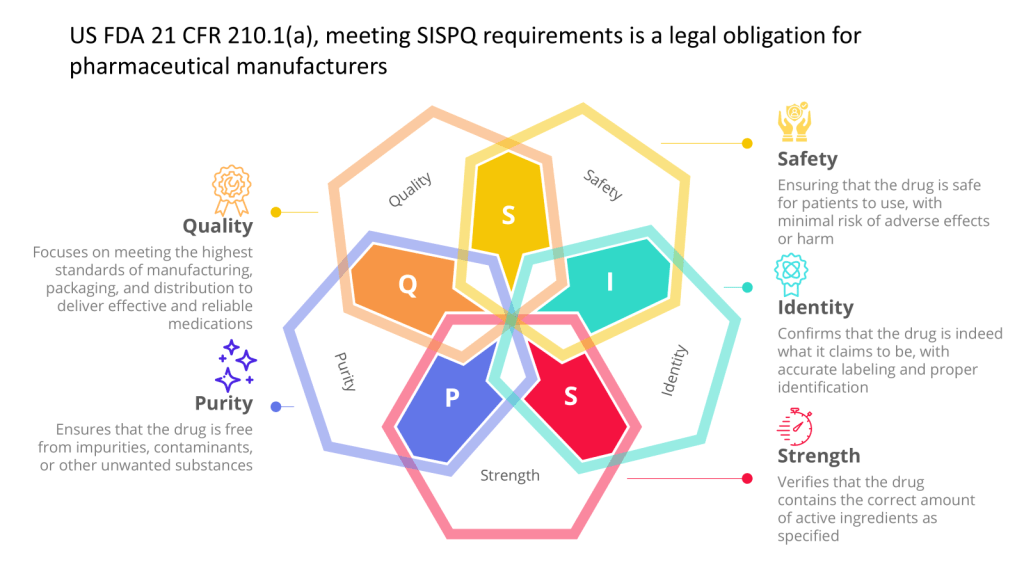
Twenty hair contamination deviations. Seven months to notify suppliers. Critical equipment failures dismissed as “not impacting SISPQ.” Media fill programs missing the very interventions they should validate. This isn’t random bad luck—it’s a quality system that has systematically normalized exactly the kinds of deviations that create inspection findings.
The Architecture of Inevitable Failure
Reading through the six major observations, three systemic patterns emerge that align perfectly with the hidden architecture of failure I discussed in my recent post on zemblanity.
Pattern 1: Investigation Theatre Over Causal Understanding
Observation 1 reveals what happens when investigations become compliance exercises rather than learning tools. The hair contamination trend—20 deviations spanning multiple product codes—received investigation resources proportional to internal requirement, not actual risk. As I’ve written about causal reasoning versus negative reasoning, these investigations focused on what didn’t happen rather than understanding the causal mechanisms that allowed hair to systematically enter sterile products.
The tribal knowledge around plunger seating issues exemplifies this perfectly. Operators developed informal workarounds because the formal system failed them, yet when this surfaced during an investigation, it wasn’t captured as a separate deviation worthy of systematic analysis. The investigation closed the immediate problem without addressing the systemic failure that created the conditions for operator innovation in the first place.
Pattern 2: Trend Blindness and Pattern Fragmentation
The most striking aspect of this 483 is how pattern recognition failed across multiple observations. Twenty-three work orders on critical air handling systems. Ten work orders on a single critical water system. Recurring membrane failures. Each treated as isolated maintenance issues rather than signals of systematic degradation.
This mirrors what I’ve discussed about normalization of deviance—where repeated occurrences of problems that don’t immediately cause catastrophe gradually shift our risk threshold. The work orders document a clear pattern of equipment degradation, yet each was risk-assessed as “not impacting SISPQ” without apparent consideration of cumulative or interactive effects.
Pattern 3: Control System Fragmentation
Perhaps most revealing is how different control systems operated in silos. Visual inspection systems that couldn’t detect the very defects found during manual inspection. Environmental monitoring that didn’t include the most critical surfaces. Media fills that omitted interventions documented as root causes of previous failures.
This isn’t about individual system inadequacy—it’s about what happens when quality systems evolve as collections of independent controls rather than integrated barriers designed to work together.
Solutions: From Zemblanity to Serendipity
Drawing from the approaches I’ve developed on this blog, here’s how Catalent could transform their quality system from one that breeds inevitable failure to one that creates conditions for quality serendipity:
Implement Causally Reasoned Investigations
The Energy Safety Canada white paper I discussed earlier this year offers a powerful framework for moving beyond counterfactual analysis. Instead of concluding that operators “failed to follow procedure” regarding stopper installation, investigate why the procedure was inadequate for the equipment configuration. Instead of noting that supplier notification was delayed seven months, understand the systemic factors that made immediate notification unlikely.
Practical Implementation:
- Retrain investigators in causal reasoning techniques
- Require investigation sponsors (area managers) to set clear expectations for causal analysis
- Implement structured causal analysis tools like Cause-Consequence Analysis
- Focus on what actually happened and why it made sense to people at the time
- Implement rubrics to guide consistency
Build Integrated Barrier Systems
The take-the-best heuristic I recently explored offers a powerful lens for barrier analysis. Rather than implementing multiple independent controls, identify the single most causally powerful barrier that would prevent each failure type, then design supporting barriers that enhance rather than compete with the primary control.
For hair contamination specifically:
- Implement direct stopper surface monitoring as the primary barrier
- Design visual inspection systems specifically to detect proteinaceous particles
- Create supplier qualification that includes contamination risk assessment
- Establish real-time trend analysis linking supplier lots to contamination events
Establish Dynamic Trend Integration
Traditional trending treats each system in isolation—environmental monitoring trends, deviation trends, CAPA trends, maintenance trends. The Catalent 483 shows what happens when these parallel trend systems fail to converge into integrated risk assessment.
Integrated Trending Framework:
- Create cross-functional trend review combining all quality data streams
- Implement predictive analytics linking maintenance patterns to quality risks
- Establish trigger points where equipment degradation patterns automatically initiate quality investigations
- Design Product Quality Reviews that explicitly correlate equipment performance with product quality data
Transform CAPA from Compliance to Learning
The recurring failures documented in this 483—repeated hair findings after CAPA implementation, continued equipment failures after “repair”—reflect what I’ve called the effectiveness paradox. Traditional CAPA focuses on thoroughness over causal accuracy.
CAPA Transformation Strategy:
- Implement a proper CAPA hierarchy, prioritizing elimination and replacement over detection and mitigation
- Establish effectiveness criteria before implementation, not after
- Create learning-oriented CAPA reviews that ask “What did this teach us about our system?”
- Link CAPA effectiveness directly to recurrence prevention rather than procedural compliance
Build Anticipatory Quality Architecture
The most sophisticated element would be creating what I call “quality serendipity”—systems that create conditions for positive surprises rather than inevitable failures. This requires moving from reactive compliance to anticipatory risk architecture.
Anticipatory Elements:
- Implement supplier performance modeling that predicts contamination risk before it manifests
- Create equipment degradation models that trigger quality assessment before failure
- Establish operator feedback systems that capture emerging risks in real-time
- Design quality reviews that explicitly seek weak signals of system stress
The Cultural Foundation
None of these technical solutions will work without addressing the cultural foundation that allowed this level of systematic failure to persist. The 483’s most telling detail isn’t any single observation—it’s the cumulative picture of an organization where quality indicators were consistently rationalized rather than interrogated.
As I’ve written about quality culture, without psychological safety and learning orientation, people won’t commit to building and supporting robust quality systems. The tribal knowledge around plunger seating, the normalization of recurring equipment failures, the seven-month delay in supplier notification—these suggest a culture where adaptation to system inadequacy became preferable to system improvement.
The path forward requires leadership that creates conditions for quality serendipity: reward pattern recognition over problem solving, celebrate early identification of weak signals, and create systems that make the right choice the easy choice.
Beyond Compliance: Building Anti-Fragile Quality
The Catalent 483 offers more than a cautionary tale—it provides a roadmap for quality transformation. Every observation represents an invitation to build quality systems that become stronger under stress rather than more brittle.
Organizations that master this transformation—moving from zemblanity-generating systems to serendipity-creating ones—will find that quality becomes not just a regulatory requirement but a competitive advantage. They’ll detect risks earlier, respond more effectively, and create the kind of operational resilience that turns disruption into opportunity.
The choice is clear: continue managing quality as a collection of independent compliance activities, or build integrated systems designed to create the conditions for sustained quality success. The Catalent case shows us what happens when we choose poorly. The frameworks exist to choose better.
What patterns of “inevitable failure” do you see in your own quality systems? How might shifting from negative reasoning to causal understanding transform your approach to investigations? Share your thoughts—this conversation about quality transformation is one we need to have across the industry.